Männliche Reproduktionspathologie
3
Produkte
Sortierung:
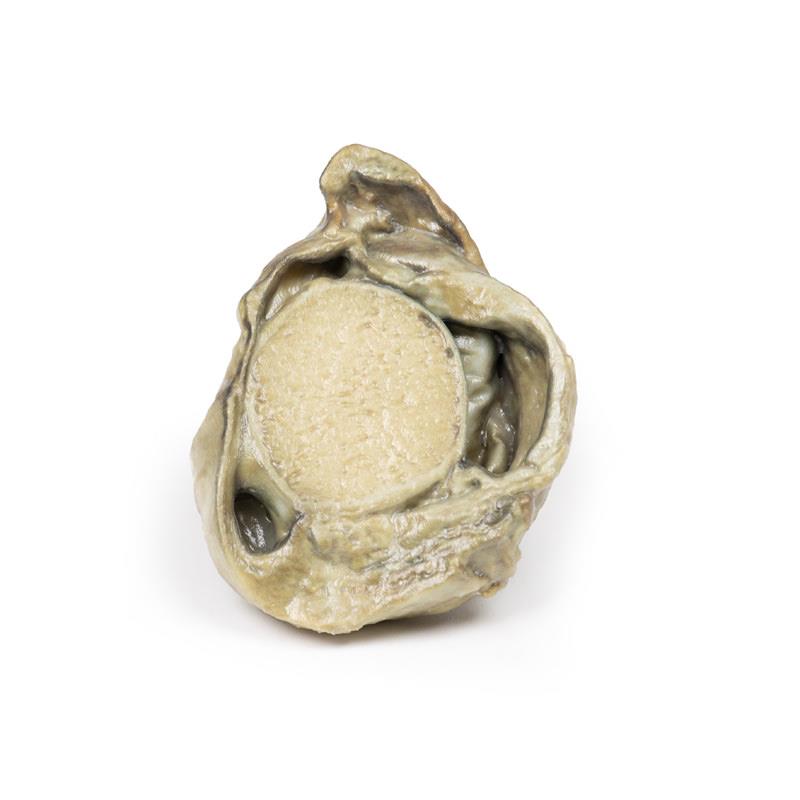
Nodular hyperplasia of the Prostate
180,88 €*
Clinical HistoryA 63-year old male presented to the emergency departed with acute abdominal pain. He has been unable to pass urine for 5 days. Further questioning revealed a 2-year history of urinary frequency, double void, urinary hesitancy, nocturia and a poor urine stream. Abdominal examination showed a tender distended bladder and an enlarged palpable prostate on digital rectal examination. A bedside bladder scan demonstrated a volume of >1L in the bladder. Blood tests shows a severe acute kidney injury. He is diagnosed with acute renal failure due to acute urinary retention. There were multiple failed attempts at catheterising the patient via the urethra and suprapublically. A total prostatectomy was performed and he made a good recovery.Pathology The specimen is an enlarged prostate gland sliced transversely to display the external and cut surfaces, On the cut surface there are numerous nodules varying in size from 2-10mm in diameter. This is an example of benign nodular hyperplasia (BPH) of the prostate gland.Note Benign prostatic hyperplasia (BPH) or nodular hyperplasia of the prostate is a common disease in older men. BPH is caused by nodular hyperplasia of prostatic stromal and glandular epithelial cells primarily in the periurethral prostate. Hyperplasia is a result of accumulation of senescent cells due to impaired cell death and cell proliferation driven by androgens, mainly dihydrotesterone. Disproportionate enlargement of the median lobe is a common feature of nodular hyperplasia of the prostate. The projecting median lobe may occlude the internal urethral orifice on contraction of the bladder.Prevalence of BPH increases significantly with age. BPH is present in 20% of males at 40 years of age, 70% of males of 60 year of age and almost 90% of males by the age of 80. There is an increased risk of BPH in men with a positive family history of BPH, in obese males and exposure to exogenous androgenic-anabolic steroids.Clinical presentation of BPH results from urinary obstructive symptoms. Patients complain of urinary frequency, nocturia, urinary hesitancy, double voiding, poor urinary stream and overflow dribbling. Acute urinary retention may result from complete urinary tract obstruction as in the case discussed above. Post void residual urine results from the obstructing prostate which leads to an increased risk of urinary tract infections.Diagnosis can be made on clinical history and physical examination of the prostate with a digital rectal exam. Prostate specific antigen may be used to screen for prostate cancer. Ultrasound scan or CT can be used to evaluate the volume of the prostate. Treatment of BPH can be treated medically with Alpha-blockers to relax the prostate smooth muscle tone or 5-alpha-reductase inhibitors, which inhibit synthesis of dihydrotesterone. The main surgical treatment for severe cases of BPH is transurethral resection of the prostate (TURP). Total prostatectomy is no longer used due to risk of disabling complications.
Hydrocoele
172,55 €*
Clinical HistoryA 40-year old male presents with shortness of breath and swelling of his lower limbs. He is a smoker with a history of diabetes and previous myocardial infarctions. On examination bilateral pleural effusion, peripheral pitting oedema and a swollen scrotum were noted. Transillumination of the swelling transmitted red light. Chest x-ray showed radiological features of congestive cardiac failure. He was commenced on appropriate treatment for heart failure but later died during this admission.PathologyThe specimen is a testis and its coverings, sliced to display the cut surface. The cavity bounded by the visceral and parietal layers of the tunica vaginalis is distended due to the accumulation of serous fluid. This is an example of a hydrocoele, secondary to generalised oedema due to congestive cardiac failure.Further InformationA hydrocele is an accumulation of serous fluid between the parietal and visceral layers of the tunica vaginalis around the testes. Hydroceles can be described as communicating with the peritoneal cavity or non-communicating with the peritoneal cavity.Communicating hydroceles develop as a result of failure of the processus vaginalis to close after the descent of the testes into the scrotum. These may present after birth as a congenital hydrocele or may present later in life due to increase in intra-abdominal pressure, such a cardiac failure in this case. Non-communicating hydroceles are caused by imbalances in fluid secretion and reabsorption e.g. orchitis, epididymitis, testicular tumour, physical trauma (e.g. hernia, testicular torsion) or defective lymphatic drainage (e.g. filariasis, elephantiasis).Patients present with a scrotal mass. The mass may be uni- or bilateral. Communicating hydroceles may be reducible and increase in size with raised intra-abdominal pressure. Non-communicating are usually non-reducible swellings. The swelling is usually non tender unless there is an underlying infection or torsion causing the hydrocele. Larger hydroceles may be cumbersome and cause erosion and skin infections on the scrotum. Diagnosis can be made on physical examination. Serous fluid allows the passage of light shined through the scrotum when examined: this is called transillumination. Ultrasound may be used to consolidate diagnosis and exclude other testicular pathology. Testicular cancer serum markers, such as alpha fetoprotein and B-HCG, may be taken to exclude testicular cancer.Many congenital hydroceles resolve spontaneously before the age of 2. If communicating hydroceles persist beyond 2 year they are surgically repaired in order to reduce the risk of developing incarcerated hernias. Surgical repair of communicating hydroceles in older patients may be offered if they are symptomatic. Treatment of the underlying aetiology of reactive hydrocele may cause them to resolve.
Chronic hydrocoele
248,71 €*
Clinical HistoryAn 80-year old male presented with haematemesis. He has a known history of alcoholic liver cirrhosis with oesophageal varices. On examination, he is noted to have multiple spider naevi, large volume abdominal ascites and a scrotal swelling. Transillumination of the swelling transmitted red light. He experienced another large volume haematemesis and died shortly after admission.Pathology The specimen consists of a testis, tunica vaginalis and distal end of the spermatic cord. The testis and its surrounding layers have been bisected to display the cut surface. The tunica vaginalis is thickened and the enclosed cavity is distended. The testis is normal. This is an example of a chronic secondary communicated hydrocoele.Further InformationA hydrocele is an accumulation of serous fluid between the parietal and visceral layers of the tunica vaginalis around the testes. Hydroceles can be described as communicating with the peritoneal cavity or non-communicating with the peritoneal cavity.Communicating hydroceles develop due to failure of the processus vaginalis to close after the descent of the testes into the scrotum. These may present after birth as a congenital hydrocele or may present later in life due to increase in intra-abdominal pressure such a cardiac failure in this case. Non-communicating hydroceles are caused by imbalances in fluid secretion and reabsorption (e.g. orchitis, epididymitis), testicular tumour, physical trauma (e.g. hernia, testicular torsion) or defective lymphatic drainage (e.g. filariasis, elephantiasis).Patients present with a scrotal mass. The mass may be uni- or bilateral. Communicating hydroceles may be reducible and increase in size with raised intra-abdominal pressure. Non-communicating are usually non-reducible swellings. The swelling is usually non tender unless there is an underlying infection or torsion causing the hydrocele. Larger hydroceles may be cumbersome and cause erosion and skin infections on the scrotum.Diagnosis can be made on physical examination. Serous fluid allows the passage of light shined through the scrotum when examined: this is called transillumination. Ultrasound may be used to consolidate diagnosis and exclude other testicular pathology. Testicular cancer serum markers, such as alpha fetoprotein and B-HCG, may be taken to exclude testicular cancer.Many congenital hydroceles resolve spontaneously before the age of 2. If communicating hydroceles persist beyond 2 year they are surgically repaired due to the risk of developing incarcerated hernias. Surgical repair of communicating hydroceles in older patients may be offered if they are symptomatic. Treatment of the underlying aetiology of reactive hydrocele may cause them to resolve.
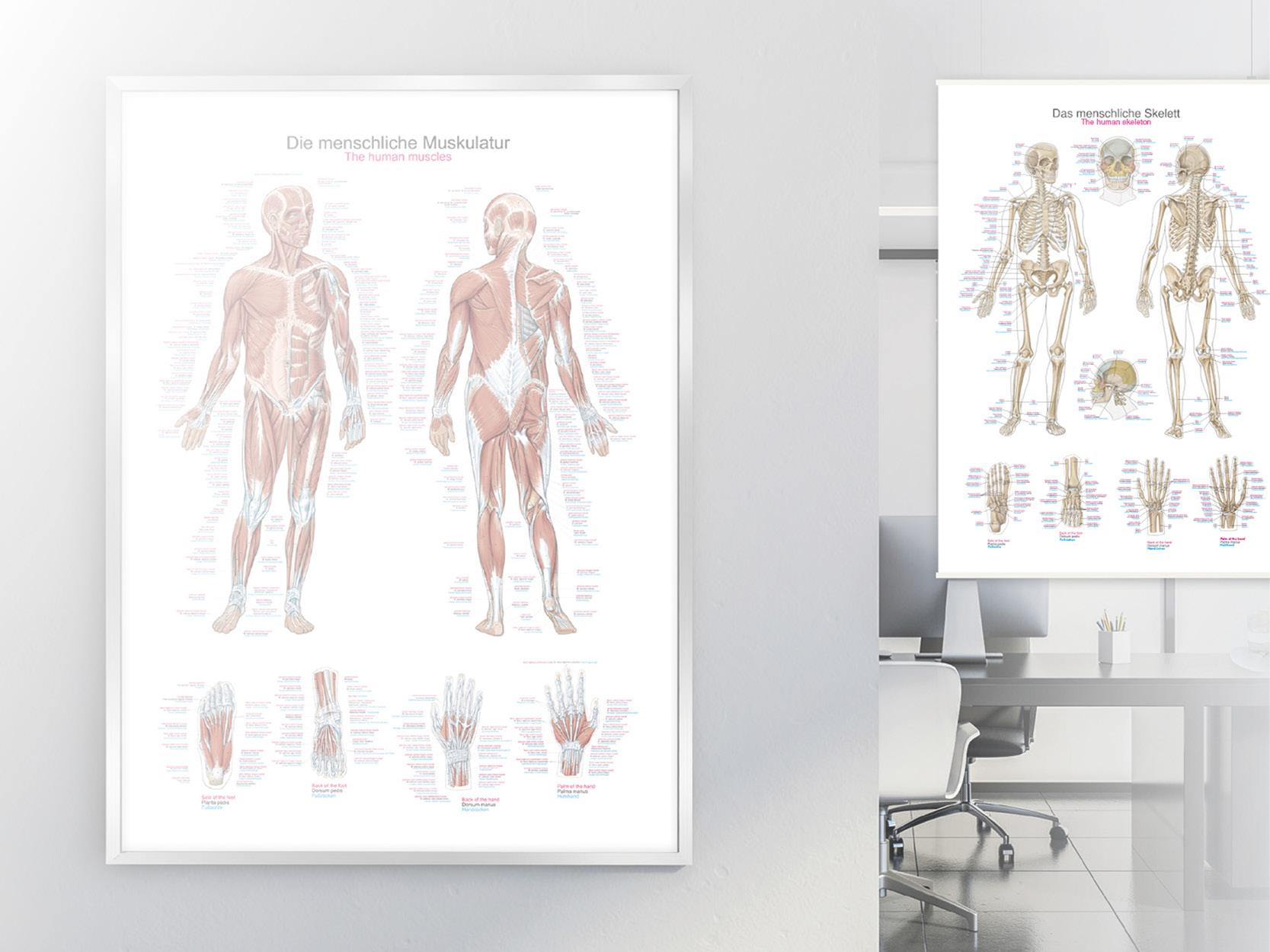
Menschliche Körperrepliken, um die Lehre zu verbessern!
Die bahnbrechende Anatomie Serie von Erler- Zimmer beinhaltet eine einzigartige und unerreichte Sammlung von kolorierten menschlichen Körperrepliken welche speziell entworfen wurden, um die Lehre und das Lernen zu verbessern. Diese Premiumkollektion von höchst akkurater humaner Anatomie wurde direkt aus radiologischen Daten oder echten Präparaten mit neuesten Bildgebenden Verfahren erzeugt. Die 3D menschliche Anatomie Serie bietet einen kosteneffektiven Weg, um Ihrem speziellen Unterrichts- und Demonstrationsbedarf im gesamten curricularen Bereich der Medizin, Gesundheitswissenschaften und der Biologie gerecht zu werden. Eine detaillierte Beschreibung der Anatomie, welche in jedem 3D-gedruckten Präparat dargestellt wird, wir mitgeliefert. Welche Vorteile bietet die Monash 3D Anatomie Serie im Vergleich zu Plastikmodellen oder echten menschlichen Plastinaten?
Jede Körperreplik wurde sorgfältig entwickelt aus ausgewählten radiologischen Patientendaten oder präparierten menschlichen Körpern höchster Qualität, welche von einem hochqualifizierten Anatomenteam im Lehrzentrum für menschliche Anatomie der Monash Universität ausgewählt wurden, um klinisch wichtige Bereiche der Anatomie in einer Qualität und Detailtreue darzustellen, wie es mit konventionellen Modellen nicht möglich ist – es handelt sich um echte Anatomie, nicht um stilisierte.
Jede Körperreplik wurde strengstens überprüft vom hochqualifizierten Anatomenteam im Lehrzentrum für menschliche Anatomie der Monash Universität, um die anatomische Genauigkeit des Endprodukts zu gewährleisten. Die Körperrepliken sind kein echtes menschliches Gewebe und unterliegen deshalb keinen Einschränkungen beim Transport, Import oder der Verwendung in Bildungseinrichtungen, die keine Erlaubnis zur Verwendung von Leichen haben. Die
Die exklusive 3D Anatomie Serie vermeidet diese und andere ethische Probleme, welche auftreten, wenn man mit plastinierten menschlichen Überresten umgeht.