Produktinformationen "Cerebral Arterio-Venous Malformation"
Klinische Vorgeschichte
Der 58-jährige Patient verstarb an postoperativen Komplikationen nach einer transurethralen Resektion der Prostata. Bereits mit 28 und 35 Jahren hatte er vorübergehende neurologische Ausfälle. Mit 50 entwickelte er eine permanente Hemiparese des linken Beins, insbesondere im Bereich des Sprunggelenks.
Pathologie
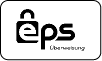
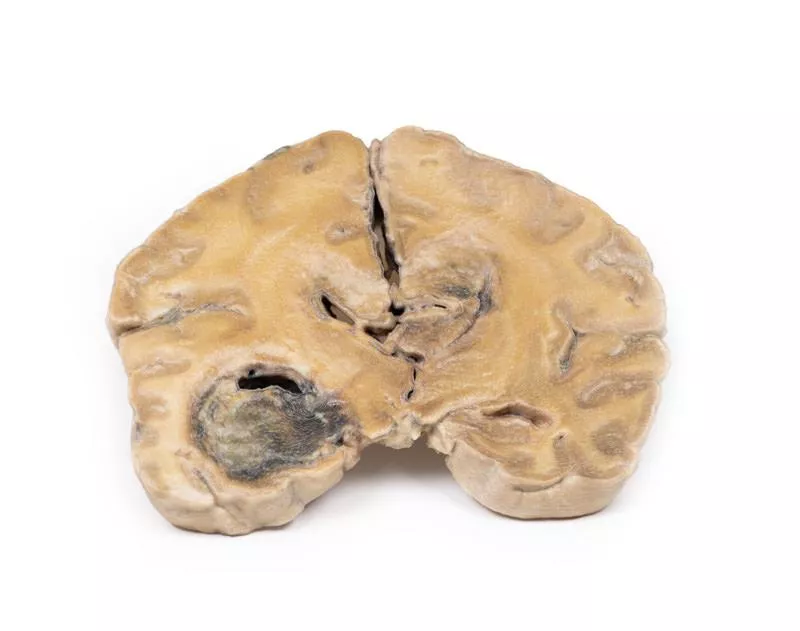
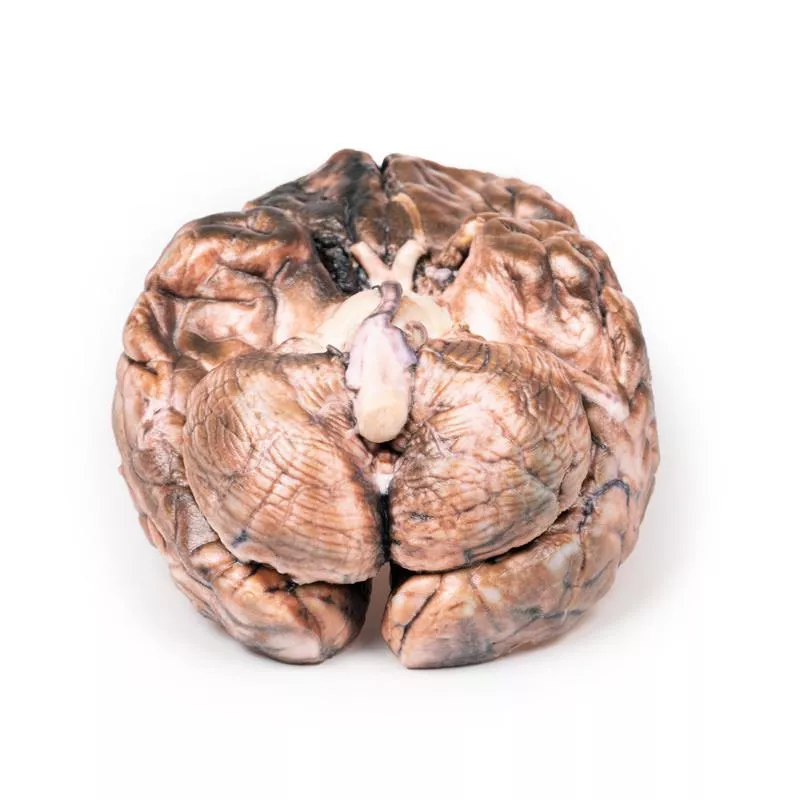
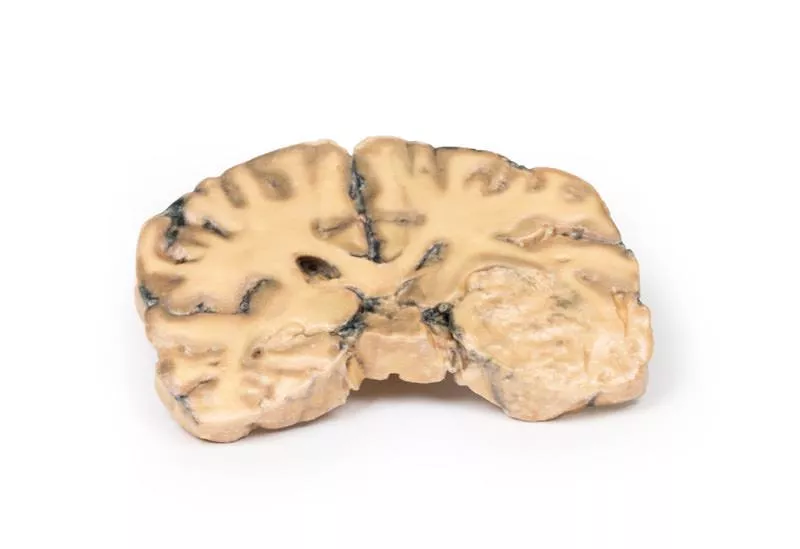
Die koronale Hirnscheibe durch die Parietallappen zeigt eine 4 cm große Läsion in der medialen rechten Hemisphäre, die sich vom Kortex bis zur Seitenventrikeldecke erstreckt. Das Gewebe besteht aus einem Netzwerk geschlängelter Gefäßkanäle. Histologisch wurde eine arteriovenöse Malformation (AVM) mit glialem Gewebe und dilatierten Arterien und Venen bestätigt.
Weitere Informationen
Zerebrale AVMs können Symptome wie Kopfschmerzen, Krampfanfälle und Hirnnervenausfälle verursachen, bleiben aber manchmal unbemerkt. Bei einem Gefäßriss kann es zu Hirnblutungen kommen mit Symptomen wie Bewusstlosigkeit, Übelkeit, Erbrechen und Sehstörungen. Je nach Ort der Blutung sind einseitige Lähmungen (Hemiparese) oder Sprachstörungen (Aphasie) möglich. Rupturierte AVMs gehen mit hoher Sterblichkeit und Langzeitfolgen einher.
Der 58-jährige Patient verstarb an postoperativen Komplikationen nach einer transurethralen Resektion der Prostata. Bereits mit 28 und 35 Jahren hatte er vorübergehende neurologische Ausfälle. Mit 50 entwickelte er eine permanente Hemiparese des linken Beins, insbesondere im Bereich des Sprunggelenks.
Pathologie
Die koronale Hirnscheibe durch die Parietallappen zeigt eine 4 cm große Läsion in der medialen rechten Hemisphäre, die sich vom Kortex bis zur Seitenventrikeldecke erstreckt. Das Gewebe besteht aus einem Netzwerk geschlängelter Gefäßkanäle. Histologisch wurde eine arteriovenöse Malformation (AVM) mit glialem Gewebe und dilatierten Arterien und Venen bestätigt.
Weitere Informationen
Zerebrale AVMs können Symptome wie Kopfschmerzen, Krampfanfälle und Hirnnervenausfälle verursachen, bleiben aber manchmal unbemerkt. Bei einem Gefäßriss kann es zu Hirnblutungen kommen mit Symptomen wie Bewusstlosigkeit, Übelkeit, Erbrechen und Sehstörungen. Je nach Ort der Blutung sind einseitige Lähmungen (Hemiparese) oder Sprachstörungen (Aphasie) möglich. Rupturierte AVMs gehen mit hoher Sterblichkeit und Langzeitfolgen einher.
Erler-Zimmer
Erler-Zimmer GmbH & Co.KG
Hauptstrasse 27
77886 Lauf
Germany
info@erler-zimmer.de
Achtung! Medizinisches Ausbildungsmaterial, kein Spielzeug. Nicht geeignet für Personen unter 14 Jahren.
Attention! Medical training material, not a toy. Not suitable for persons under 14 years of age.