Product information "Abdominal Aortic Aneurysm"
Clinical History
This 70-year-old man with a history of mild gastro-oesophageal reflux suddenly developed severe upper abdominal pain radiating to the left shoulder tip. On examination, he was distressed and hyperventilating, with a pulse rate of 87/min and blood pressure 140/90 mmHg. Abdominal exam showed board-like rigidity and reduced bowel sounds. Emergency laparotomy revealed no ruptured viscus; the pancreas appeared normal, but an unruptured abdominal aortic aneurysm was noted. Endoscopy the next day identified a ruptured oesophageal ulcer, and a Celestin tube was placed. Despite treatment, he developed localized infection, pulmonary oedema, and congestion, dying 19 days after admission.
Pathology
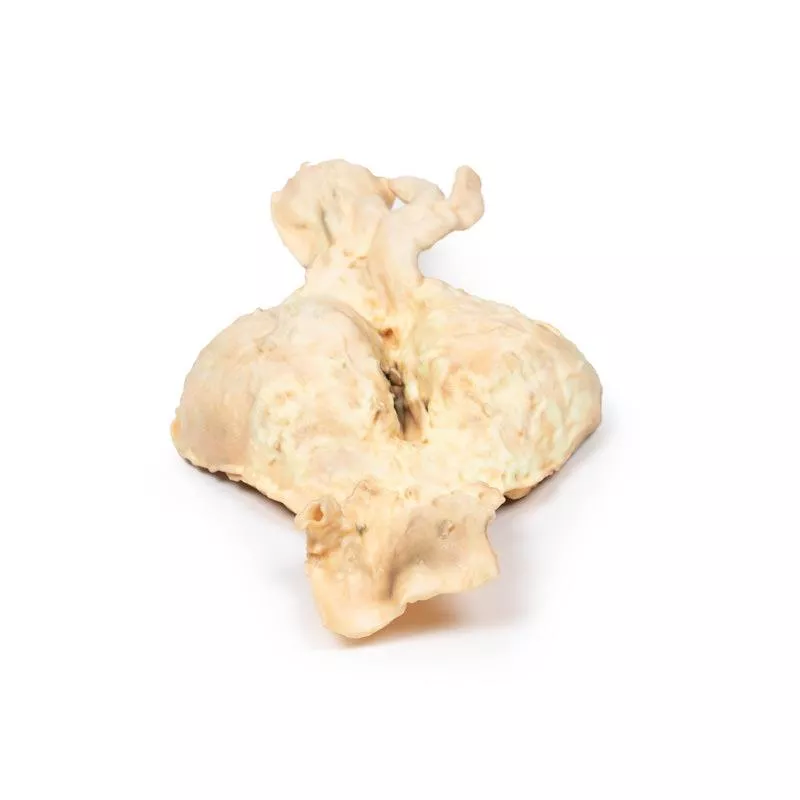
The specimen shows the lower abdominal aorta, common iliac vessels, and proximal iliac arteries. A large 10 x 7 cm aneurysm lies below the renal arteries, extending to the aortic bifurcation. The aneurysm wall is severely thinned and partly lined by laminated thrombus, indicating chronicity. Recent thrombus formation is also evident. There is aneurysmal dilatation of the common iliac and left external iliac arteries. Multiple focally ulcerated atheromatous plaques are present at the upper aorta. No rupture is seen.
Further Information
An abdominal aortic aneurysm (AAA) is a localized enlargement of the abdominal aorta (diameter >3 cm or >50% larger than normal). Most AAAs are asymptomatic unless ruptured. Large aneurysms may be palpable, and sometimes abdominal, back, or leg pain occurs. Rupture causes sudden abdominal/back pain, low blood pressure, unconsciousness, and often death. AAAs mainly affect men over 50, especially smokers or those with high blood pressure or family history. Genetic conditions like Marfan’s and Ehlers-Danlos syndromes also increase risk. About 85% of AAAs occur below the kidneys, making them the most common aortic aneurysm.
This 70-year-old man with a history of mild gastro-oesophageal reflux suddenly developed severe upper abdominal pain radiating to the left shoulder tip. On examination, he was distressed and hyperventilating, with a pulse rate of 87/min and blood pressure 140/90 mmHg. Abdominal exam showed board-like rigidity and reduced bowel sounds. Emergency laparotomy revealed no ruptured viscus; the pancreas appeared normal, but an unruptured abdominal aortic aneurysm was noted. Endoscopy the next day identified a ruptured oesophageal ulcer, and a Celestin tube was placed. Despite treatment, he developed localized infection, pulmonary oedema, and congestion, dying 19 days after admission.
Pathology
The specimen shows the lower abdominal aorta, common iliac vessels, and proximal iliac arteries. A large 10 x 7 cm aneurysm lies below the renal arteries, extending to the aortic bifurcation. The aneurysm wall is severely thinned and partly lined by laminated thrombus, indicating chronicity. Recent thrombus formation is also evident. There is aneurysmal dilatation of the common iliac and left external iliac arteries. Multiple focally ulcerated atheromatous plaques are present at the upper aorta. No rupture is seen.
Further Information
An abdominal aortic aneurysm (AAA) is a localized enlargement of the abdominal aorta (diameter >3 cm or >50% larger than normal). Most AAAs are asymptomatic unless ruptured. Large aneurysms may be palpable, and sometimes abdominal, back, or leg pain occurs. Rupture causes sudden abdominal/back pain, low blood pressure, unconsciousness, and often death. AAAs mainly affect men over 50, especially smokers or those with high blood pressure or family history. Genetic conditions like Marfan’s and Ehlers-Danlos syndromes also increase risk. About 85% of AAAs occur below the kidneys, making them the most common aortic aneurysm.
Erler-Zimmer
Erler-Zimmer GmbH & Co.KG
Hauptstrasse 27
77886 Lauf
Germany
info@erler-zimmer.de
Achtung! Medizinisches Ausbildungsmaterial, kein Spielzeug. Nicht geeignet für Personen unter 14 Jahren.
Attention! Medical training material, not a toy. Not suitable for persons under 14 years of age.