Product information "Cerebral Haemorrhage, secondary to Acute Myeloid Leukaemia"
Clinical History
A 22-year-old male presented with a two-week history of malaise, weight loss and unexplained bruising. He later developed productive cough and fever. Shortly after hospital admission for further tests, he suddenly lost consciousness and died within minutes.
Pathology
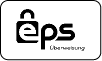
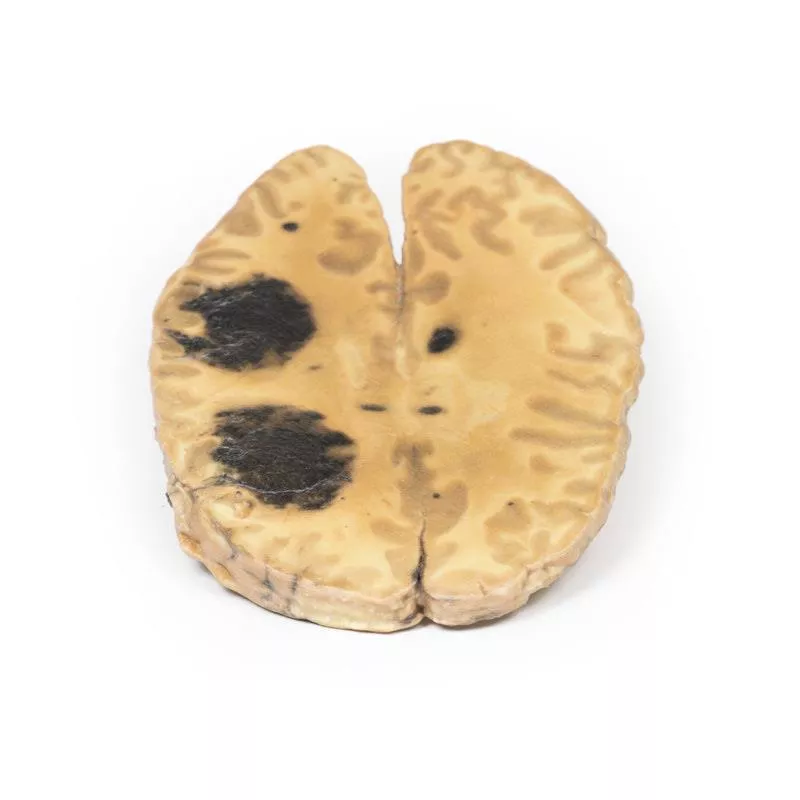
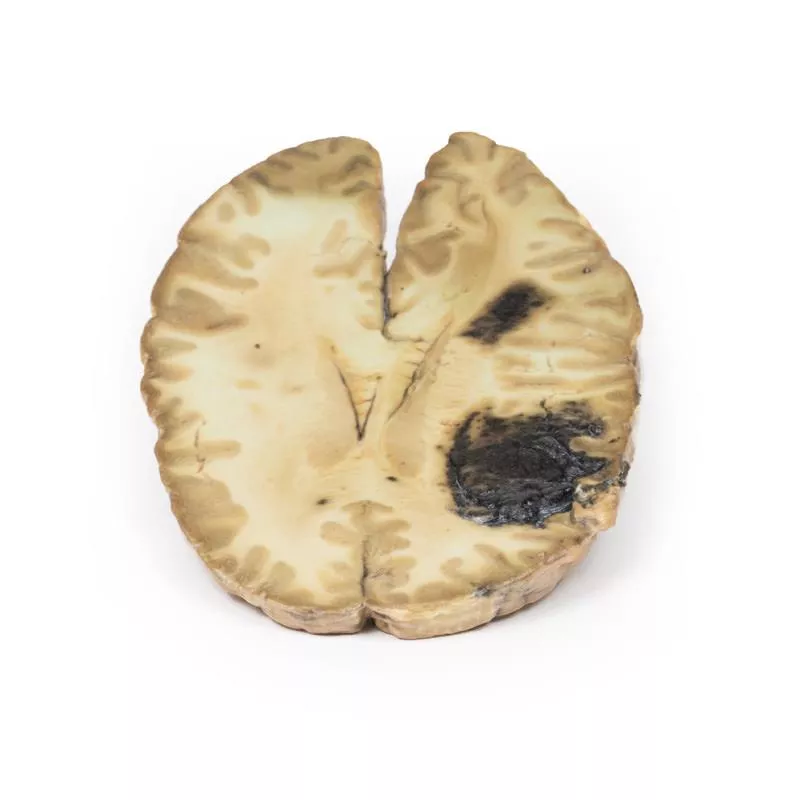
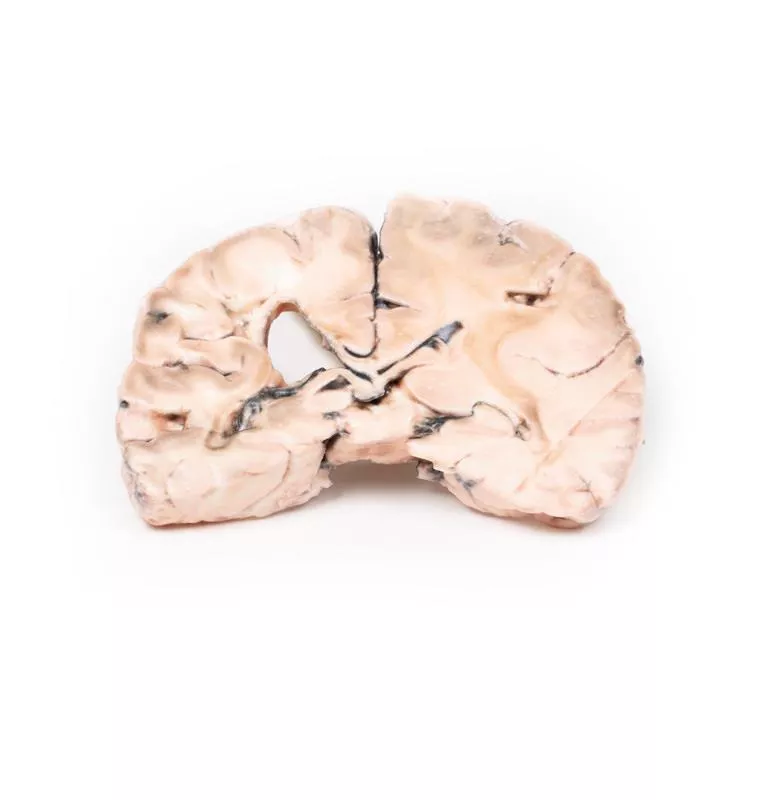
This horizontal brain section shows the superior surface with two large haemorrhages in the right frontal and parietal lobes (each approx. 5 cm), as well as multiple smaller haemorrhages in the white matter bilaterally. This presentation is consistent with multiple intraparenchymal haemorrhages in a patient with acute myeloid leukaemia (AML).
Further Information
Intraparenchymal brain haemorrhages result from rupture of small blood vessels in the brain and often present with sudden neurological decline. In AML, bone marrow failure due to immature blast accumulation leads to thrombocytopaenia, increasing the risk of spontaneous bleeding. Intracranial haemorrhage is the second most common cause of death in AML after infection. A severe bleeding disorder, disseminated intravascular coagulation (DIC), can also occur. Treatment options depend on the severity and may include haematoma evacuation, seizure control and management of intracranial pressure. Mortality for intracerebral haemorrhage is high, especially within the first 48 hours.
A 22-year-old male presented with a two-week history of malaise, weight loss and unexplained bruising. He later developed productive cough and fever. Shortly after hospital admission for further tests, he suddenly lost consciousness and died within minutes.
Pathology
This horizontal brain section shows the superior surface with two large haemorrhages in the right frontal and parietal lobes (each approx. 5 cm), as well as multiple smaller haemorrhages in the white matter bilaterally. This presentation is consistent with multiple intraparenchymal haemorrhages in a patient with acute myeloid leukaemia (AML).
Further Information
Intraparenchymal brain haemorrhages result from rupture of small blood vessels in the brain and often present with sudden neurological decline. In AML, bone marrow failure due to immature blast accumulation leads to thrombocytopaenia, increasing the risk of spontaneous bleeding. Intracranial haemorrhage is the second most common cause of death in AML after infection. A severe bleeding disorder, disseminated intravascular coagulation (DIC), can also occur. Treatment options depend on the severity and may include haematoma evacuation, seizure control and management of intracranial pressure. Mortality for intracerebral haemorrhage is high, especially within the first 48 hours.
Erler-Zimmer
Erler-Zimmer GmbH & Co.KG
Hauptstrasse 27
77886 Lauf
Germany
info@erler-zimmer.de
Achtung! Medizinisches Ausbildungsmaterial, kein Spielzeug. Nicht geeignet für Personen unter 14 Jahren.
Attention! Medical training material, not a toy. Not suitable for persons under 14 years of age.