Product information "Intracranial space-occupying lesion"
Clinical History
A 56-year-old woman with a 6-month history of intermittent headaches and vomiting was admitted to hospital in a comatose state following a grand mal seizure. She did not regain consciousness.
Pathology
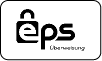
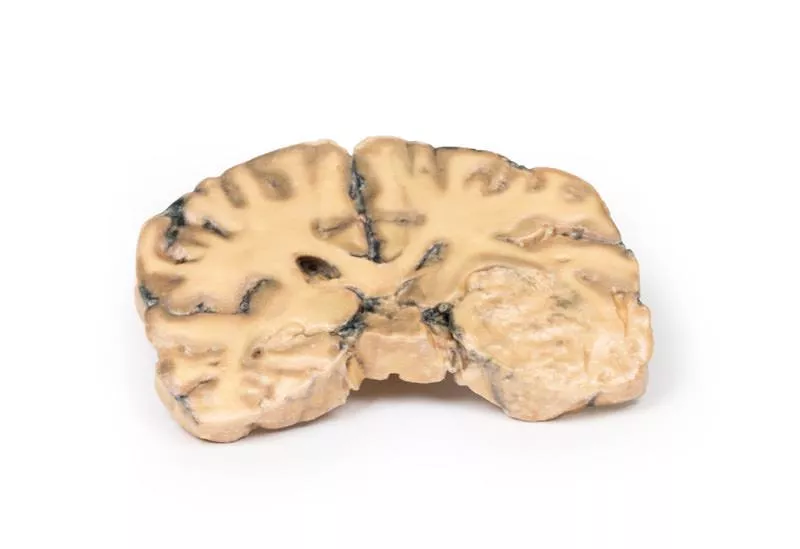
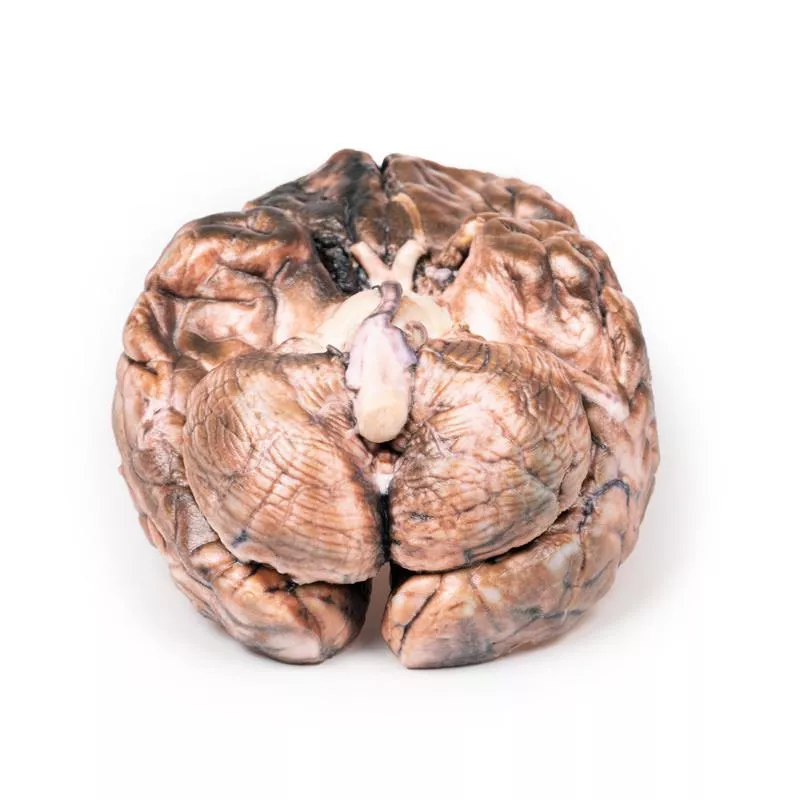
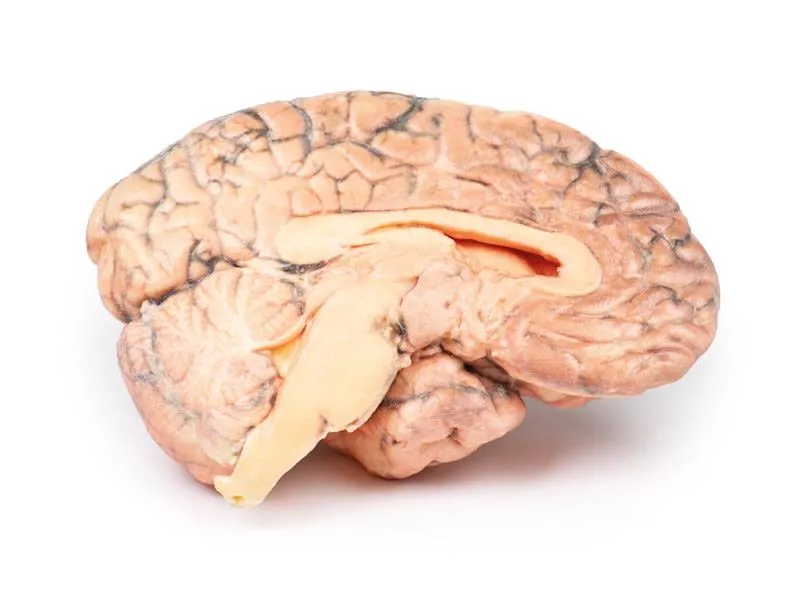
This coronal brain section reveals that the brain has been compressed laterally and downward due to a large intracranial mass on the right side, likely a meningioma (though the tumour itself is not present in the section). The anterior view shows a midline shift with subfalcine herniation of the cingulate gyrus. The posterior view displays haemorrhages of varying ages in the temporal lobe and pons, which are typical for a supratentorial mass lesion. There is also noticeable ventricular asymmetry.
Further Information
A space-occupying meningioma can exert pressure on brain tissue, resulting in atrophy and displacement, which in turn may affect cranial nerve function, blood flow, and normal brain processes. Common symptoms may include:
- Seizures – such as myoclonic (brief muscle jerks or spasms) or tonic-clonic (loss of consciousness, muscle rigidity, followed by convulsions and potential loss of body control).
- Sensory disturbances – changes in vision, smell, or hearing without loss of consciousness.
The presentation can vary depending on the tumour’s location.
A 56-year-old woman with a 6-month history of intermittent headaches and vomiting was admitted to hospital in a comatose state following a grand mal seizure. She did not regain consciousness.
Pathology
This coronal brain section reveals that the brain has been compressed laterally and downward due to a large intracranial mass on the right side, likely a meningioma (though the tumour itself is not present in the section). The anterior view shows a midline shift with subfalcine herniation of the cingulate gyrus. The posterior view displays haemorrhages of varying ages in the temporal lobe and pons, which are typical for a supratentorial mass lesion. There is also noticeable ventricular asymmetry.
Further Information
A space-occupying meningioma can exert pressure on brain tissue, resulting in atrophy and displacement, which in turn may affect cranial nerve function, blood flow, and normal brain processes. Common symptoms may include:
- Seizures – such as myoclonic (brief muscle jerks or spasms) or tonic-clonic (loss of consciousness, muscle rigidity, followed by convulsions and potential loss of body control).
- Sensory disturbances – changes in vision, smell, or hearing without loss of consciousness.
The presentation can vary depending on the tumour’s location.
Erler-Zimmer
Erler-Zimmer GmbH & Co.KG
Hauptstrasse 27
77886 Lauf
Germany
info@erler-zimmer.de
Achtung! Medizinisches Ausbildungsmaterial, kein Spielzeug. Nicht geeignet für Personen unter 14 Jahren.
Attention! Medical training material, not a toy. Not suitable for persons under 14 years of age.