Product information "Metastatic melanoma"
Clinical History
In the 1970s, a 31-year-old woman presented with severe headache and diplopia, eight months after the removal of an invasive pigmented skin melanoma from her neck. Initial clinical examination revealed no abnormalities. She was discharged but re-admitted later with persistent vomiting. Her condition rapidly deteriorated, and she died shortly after.
Pathology
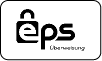
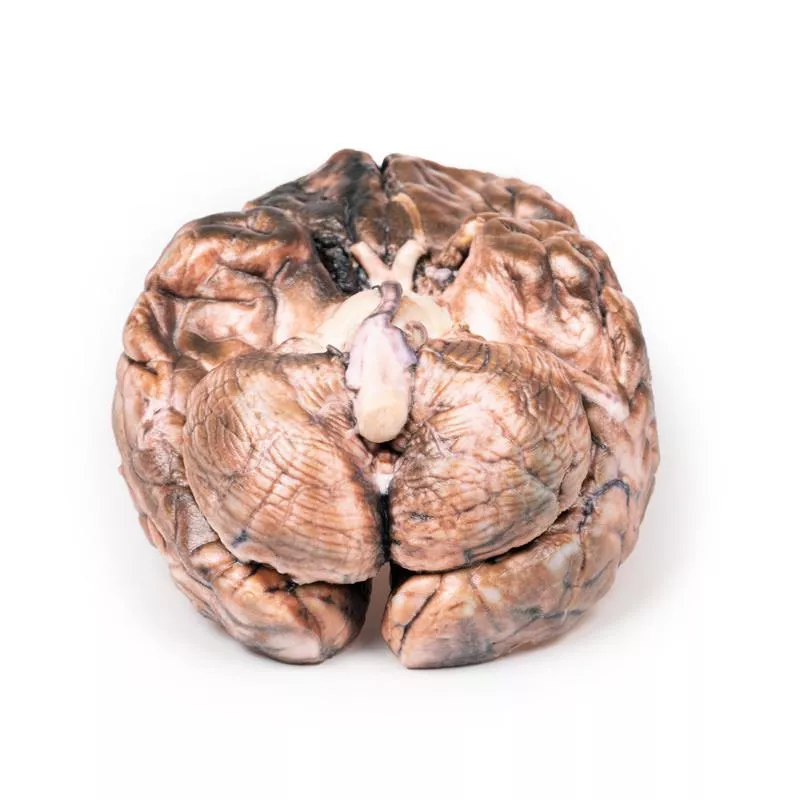
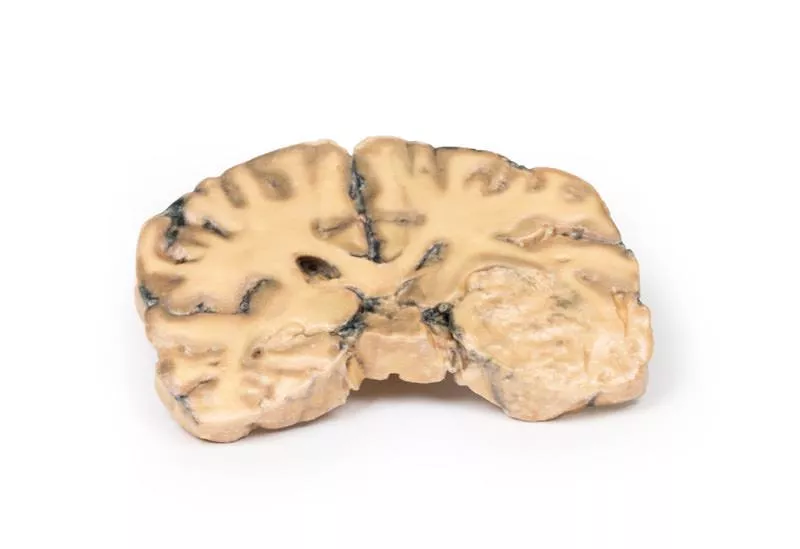
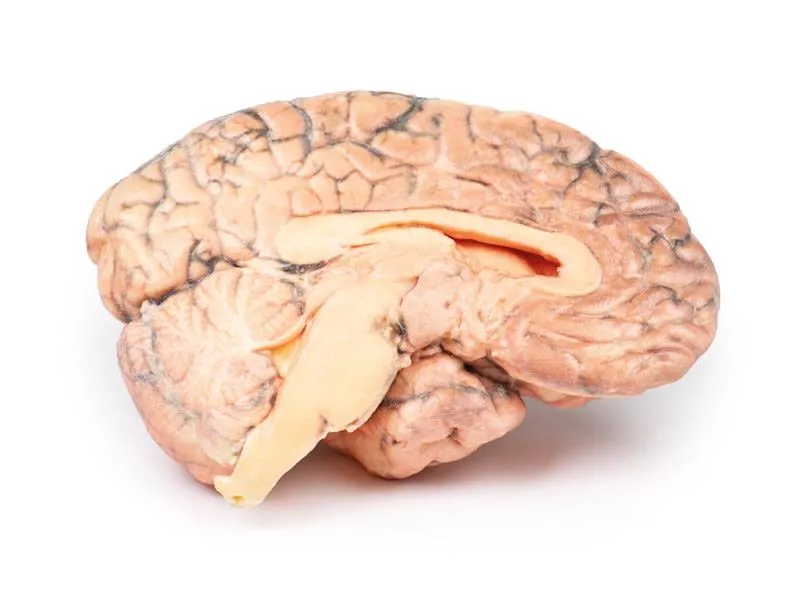
The brain specimen shows extensive intracerebral melanoma metastases. The inferior surface displays numerous dark nodules up to 1.5 cm in diameter. On the cut superior surface, similar lesions are visible and confined to the grey matter. The tumour nodules are not encapsulated and infiltrate the cortex, with areas of necrosis and haemorrhage present.
Further Information
Melanoma accounts for about 10% of all brain metastases. Risk increases with age over 60, male gender, disease progression, and certain genetic mutations such as BRAF or NRAS. Most metastases are supratentorial and may present with headache, neurological deficits or seizures. These lesions have a known risk of spontaneous haemorrhage. Diagnosis is based on imaging and histological confirmation. Treatment often involves stereotactic radiosurgery, radiotherapy, and systemic immunotherapy or targeted therapies, improving median survival to around 11 months in recent years.
In the 1970s, a 31-year-old woman presented with severe headache and diplopia, eight months after the removal of an invasive pigmented skin melanoma from her neck. Initial clinical examination revealed no abnormalities. She was discharged but re-admitted later with persistent vomiting. Her condition rapidly deteriorated, and she died shortly after.
Pathology
The brain specimen shows extensive intracerebral melanoma metastases. The inferior surface displays numerous dark nodules up to 1.5 cm in diameter. On the cut superior surface, similar lesions are visible and confined to the grey matter. The tumour nodules are not encapsulated and infiltrate the cortex, with areas of necrosis and haemorrhage present.
Further Information
Melanoma accounts for about 10% of all brain metastases. Risk increases with age over 60, male gender, disease progression, and certain genetic mutations such as BRAF or NRAS. Most metastases are supratentorial and may present with headache, neurological deficits or seizures. These lesions have a known risk of spontaneous haemorrhage. Diagnosis is based on imaging and histological confirmation. Treatment often involves stereotactic radiosurgery, radiotherapy, and systemic immunotherapy or targeted therapies, improving median survival to around 11 months in recent years.
Erler-Zimmer
Erler-Zimmer GmbH & Co.KG
Hauptstrasse 27
77886 Lauf
Germany
info@erler-zimmer.de
Achtung! Medizinisches Ausbildungsmaterial, kein Spielzeug. Nicht geeignet für Personen unter 14 Jahren.
Attention! Medical training material, not a toy. Not suitable for persons under 14 years of age.