Product information "Glioblastoma multiforme"
Clinical History
Over a 3-year period, a 57-year-old woman experienced intermittent frontal headaches and memory disturbances that progressed to psychiatric symptoms, vomiting, and meningeal signs. Localising neurological signs appeared only late in the disease course.
Pathology
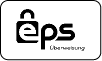
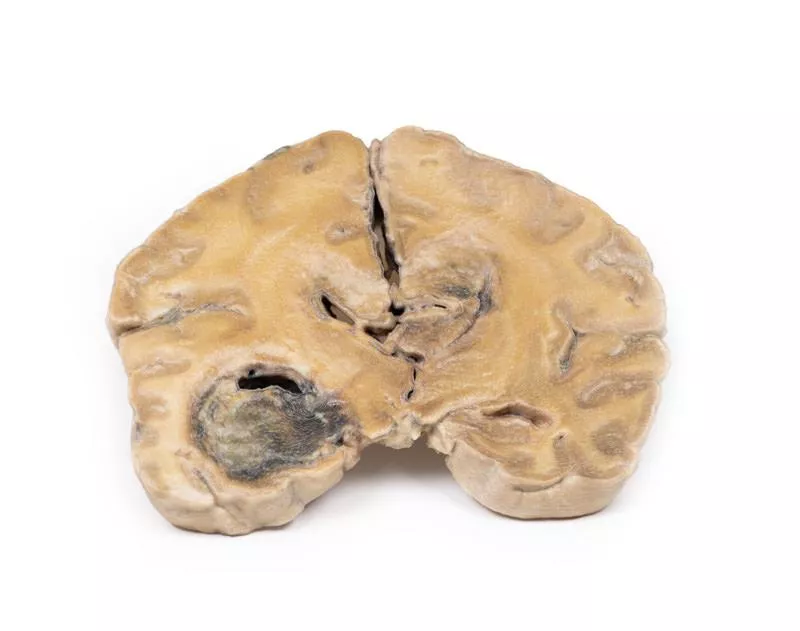
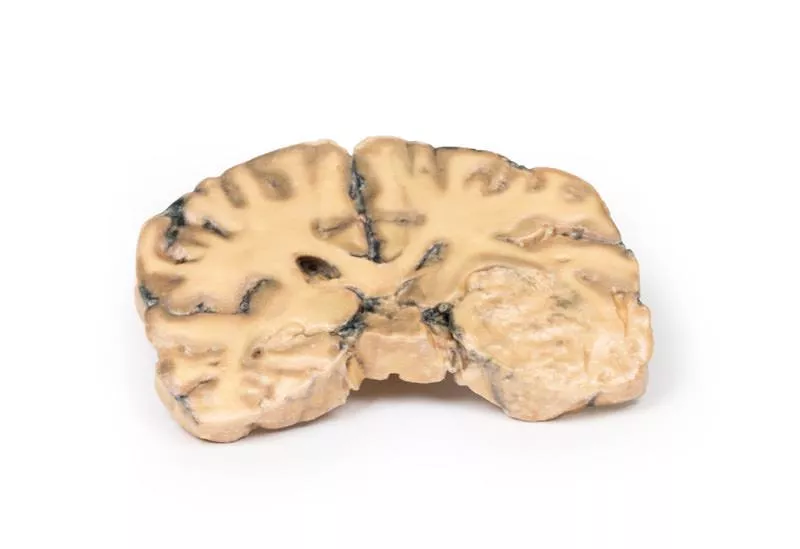
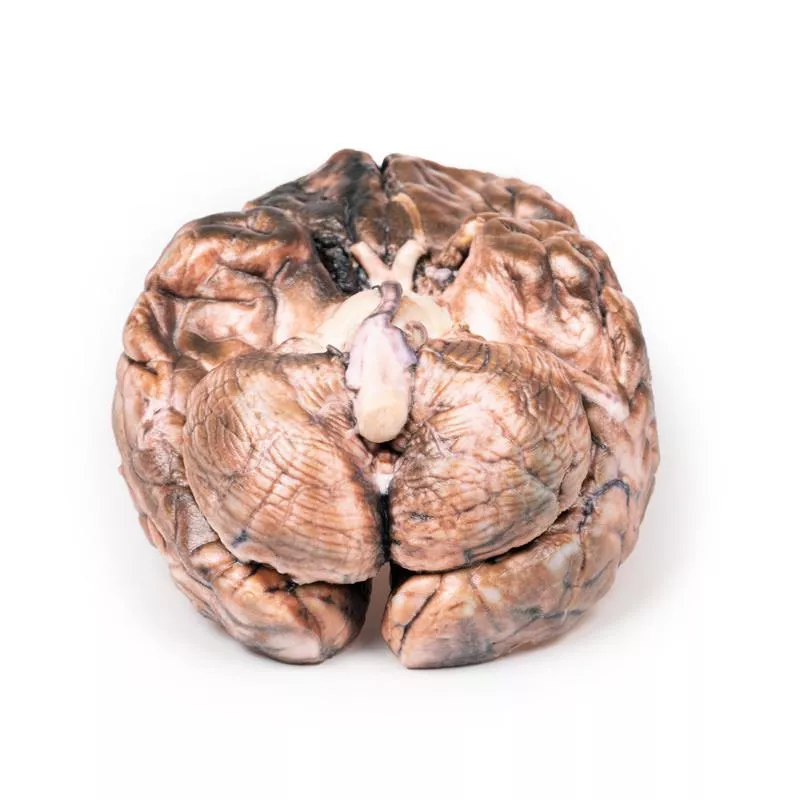
A coronal section of the cerebral hemisphere reveals a round, haemorrhagic, variegated tumour in the left temporal lobe. Tumour tissue extends across the midline, replacing the corpus callosum and nearly obliterating the ventricular system. Further sections confirmed these lesions are part of one massive tumour.
Further Information
Gliomas are the second most common CNS cancer after meningiomas. These tumours resemble normal macroglial cells—astrocytes, oligodendrocytes, and ependymal cells—and arise from progenitor cells differentiating along these lines. Glioblastoma multiforme (GBM), a grade IV astrocytoma, can develop de novo or from lower-grade gliomas. Histologically, GBMs feature necrosis surrounded by anaplastic cells and hyperplastic blood vessels. GBMs are more frequent in males and typically diagnosed in the 6th decade. Risk factors include neurofibromatosis type 1, Li-Fraumeni syndrome, and prior brain radiotherapy. Symptoms depend on tumour location and include persistent headaches, visual disturbances, vomiting, appetite loss, mood and personality changes, cognitive decline, new seizures, and speech difficulties. Diagnosis relies on CT and MRI. About 50% of GBMs involve more than one hemisphere and often invade ventricular walls or meninges, occasionally reaching the CSF. Metastases outside the CNS are rare. Tumour growth causes cerebral oedema and increased intracranial pressure. These aggressive tumours have a median survival of around 3 months if untreated. Treatment includes surgery, radiation, and chemotherapy.
Over a 3-year period, a 57-year-old woman experienced intermittent frontal headaches and memory disturbances that progressed to psychiatric symptoms, vomiting, and meningeal signs. Localising neurological signs appeared only late in the disease course.
Pathology
A coronal section of the cerebral hemisphere reveals a round, haemorrhagic, variegated tumour in the left temporal lobe. Tumour tissue extends across the midline, replacing the corpus callosum and nearly obliterating the ventricular system. Further sections confirmed these lesions are part of one massive tumour.
Further Information
Gliomas are the second most common CNS cancer after meningiomas. These tumours resemble normal macroglial cells—astrocytes, oligodendrocytes, and ependymal cells—and arise from progenitor cells differentiating along these lines. Glioblastoma multiforme (GBM), a grade IV astrocytoma, can develop de novo or from lower-grade gliomas. Histologically, GBMs feature necrosis surrounded by anaplastic cells and hyperplastic blood vessels. GBMs are more frequent in males and typically diagnosed in the 6th decade. Risk factors include neurofibromatosis type 1, Li-Fraumeni syndrome, and prior brain radiotherapy. Symptoms depend on tumour location and include persistent headaches, visual disturbances, vomiting, appetite loss, mood and personality changes, cognitive decline, new seizures, and speech difficulties. Diagnosis relies on CT and MRI. About 50% of GBMs involve more than one hemisphere and often invade ventricular walls or meninges, occasionally reaching the CSF. Metastases outside the CNS are rare. Tumour growth causes cerebral oedema and increased intracranial pressure. These aggressive tumours have a median survival of around 3 months if untreated. Treatment includes surgery, radiation, and chemotherapy.
Erler-Zimmer
Erler-Zimmer GmbH & Co.KG
Hauptstrasse 27
77886 Lauf
Germany
info@erler-zimmer.de
Achtung! Medizinisches Ausbildungsmaterial, kein Spielzeug. Nicht geeignet für Personen unter 14 Jahren.
Attention! Medical training material, not a toy. Not suitable for persons under 14 years of age.